PrEP Provider Toolkit
Advanced Topics
HIV Acquisition while on PrEP & Risk of resistance
In rare circumstances, patients may acquire an HIV infection while taking PrEP. Usually, this occurs when there are subtherapeutic drug concentrations to prevent an HIV infection, such as when there is poor adherence or acquisition during the initial week of PrEP initiation. Since these new HIV infections occur in the presence of partial drug pressure, resistance mutations may develop, which is an often-cited concern.
Although this is not a matter to be taken lightly, the resistance patterns most often caused by F/TDF (Truvada) and F/TAF (Descovy) are commonly seen and can be easily managed. (32) This is best summarized by one study that stated that we “should respect but not fear” resistance caused by oral PrEP. (33)
Parikh, & Mellors, J. W. (2016). Should we fear resistance from tenofovir/emtricitabine preexposure prophylaxis? Current Opinion in HIV & AIDS, 11(1), 49–55.
https://doi.org/10.1097/COH.0000000000000209
Tittle, Boffito, M., McOwan, A., & Whitlock, G. (2020). Antiretroviral resistance and management after pre-exposure prophylaxis. The Lancet HIV, 7(2), e84–e84.
https://doi.org/10.1016/S2352-3018(19)30404-7
Liegler, Abdel-Mohsen, M., Bentley, L. G., Atchison, R., Schmidt, T., Javier, J., Mehrotra, M., Eden, C., Glidden, D. V., McMahan, V., Anderson, P. L., Li, P., Wong, J. K., Buchbinder, S., Guanira, J. V., Grant, R. M., & iPrEx Study Team, S. T. (2014). HIV-1 drug resistance in the iPrEx preexposure prophylaxis trial. The Journal of Infectious Diseases, 210(8), 1217–1227.
https://doi.org/10.1093/infdis/jiu233
This same investigation utilized a mathematical model to predict that the number of HIV infections that can be prevented with PrEP far exceeds the number of drug-resistant infections caused by PrEP. Many analyses corroborate this. (34)
Abbas, Glaubius, R., Mubayi, A., Hood, G., & Mellors, J. W. (2013). Antiretroviral therapy and pre-exposure prophylaxis: combined impact on HIV transmission and drug resistance in South Africa. The Journal of Infectious Diseases, 208(2), 224–234.
https://doi.org/10.1093/infdis/jit150
Baggaley, Powers, K. A., & Boily, M.-C. (2011). What do mathematical models tell us about the emergence and spread of drug-resistant HIV? Current Opinion in HIV & AIDS, 6(2), 131–140.
https://doi.org/10.1097/COH.0b013e328343ad03
Gibas, van den Berg, P., Powell, V. E., & Krakower, D. S. (2019). Drug resistance during HIV pre-exposure prophylaxis. Drugs (New York, N.Y.), 79(6), 609–619.
https://doi.org/10.1007/s40265-019-01108-x
Cabotegravir is from an entirely different class of antiretroviral medication called integrase strand transfer inhibitors (INSTI). We rely heavily on INSTIs for HIV treatment and, thus, should be much more cautious. Especially since cabotegravir has a long “tail phase” where subtherapeutic drug levels allow HIV infections to take hold and develop resistance patterns. This is why current recommendations call for continued use of F/TDF (Truvada) or F/TAF (Descovy) for a year after the last cabotegravir injection. The data on this is limited and still under investigation. (35)
Landovitz, Donnell, D., Clement, M. E., Hanscom, B., Cottle, L., Coelho, L., Cabello, R., Chariyalertsak, S., Dunne, E. F., Frank, I., Gallardo-Cartagena, J. A., Gaur, A. H., Gonzales, P., Tran, H. V., Hinojosa, J. C., Kallas, E. G., Kelley, C. F., Losso, M. H., Madruga, J. V., … Sued, O. (2021). Cabotegravir for HIV prevention in cisgender men and transgender women. The New England Journal of Medicine, 385(7), 595–608.
https://doi.org/10.1056/NEJMoa2101016
Delany-Moretlwe, Hughes, J. P., Bock, P., Hunidzarira, P., Kalonji, D., Kayange, N., Makhema, J., Mandima, P., Mathew, C., Spooner, E., Mpendo, J., Mukwekwerere, P., Mgodi, N., Ntege, P. N., Nakabiito, C., Nuwagaba-Biribonwoha, H., Panchia, R., Singh, N., Farrior, J., … Marzinke, M. A. (2022). Cabotegravir for the prevention of HIV-1 in women: results from HPTN 084, a phase 3, randomised clinical trial. The Lancet (British Edition), 399(10337), 1779–1789.
https://doi.org/10.1016/S0140-6736(22)00538-4
Regardless of which PrEP medication is used, frequent testing is the most effective way to detect HIV infections as soon as possible and prevent further communal spread.
The detailed management of HIV goes beyond the purposes of this toolkit. Check with your local institution about the process of connecting patients to HIV care.
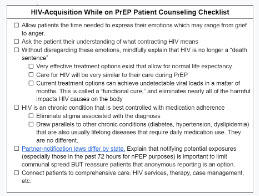
Whether or not you feel comfortable managing HIV, this is a critical time for patients to be consoled and engaged in proper care. You may be the first point of contact after a positive result.